Concerns about appearance and transmission of oral HPV infections are rising as they become more prevalent among people.
Quick exposure can occur through intimate activities like kissing or oral sex, thus, the virus become easily transmissible.
The mouth, a bustling hub of activity, can become a prime target for HPV invasion.
In the forthcoming discussion, we’ll review the visual aspects of oral HPV. Stay tuned for insights into this intriguing yet pressing matter.
What is oral HPV?
Oral HPV, short for Human Papillomavirus, refers to a group of viruses that can infect the mouth and throat. HPV is one of the most common sexually transmitted infections globally, with over 200 different types identified.
While most HPV infections resolve on their own without causing any symptoms, certain strains can lead to various health issues, including oral cancers.

In recent years, there has been a significant increase in the prevalence of oral HPV infections, particularly among young adults. This rise has prompted heightened awareness and research efforts to better understand the risks and implications associated with oral HPV transmission and infection.
HPV symptoms in the mouth
- Lesions or sores: HPV can cause the development of small, painless lesions or sores in the mouth or throat. These may appear as white or red patches, bumps, or ulcers.
- Sore throat: Those with oral HPV infections may experience persistent soreness or discomfort in the throat, which can sometimes be mistaken for a common cold or throat infection.
- Difficulty swallowing: In more advanced cases, HPV-related lesions or tumors in the throat may lead to difficulty swallowing or a sensation of something stuck in the throat.

- Changes in voice: HPV-related growths in the throat can affect vocal cord function, which will lead to changes in voice quality or hoarseness.
- Ear pain: HPV-related lesions or tumors in the throat may cause referred pain to the ears.
Does HPV in the mouth go away?
HPV infections in the mouth will go away on their own without causing any symptoms or long-term complications in some cases. Some persistent infections can lead to the development of oral cancers or other health issues.
While there is no specific treatment for HPV itself, paying more attenion to good dental hygiene, staying away tobacco and alcohol, and getting vaccinated against HPV can help reduce the risk of infection.
Best of all, regular dental check-ups and screenings can also aid in early detection and management of any oral health concerns associated with HPV. So, if you’re afriad of being infected by it, you need to check in time.
How serious is HPV in mouth?
HPV in the mouth can vary in seriousness depending on various factors, including the specific strain of the virus and individual health factors. In many cases, the infections are transient and cause no symptoms or health issues.
Sadly, infections with high-risk HPV strains, particularly HPV-16 and HPV-18, can lead to the development of oral cancers, including cancers of the throat, tongue, and tonsils.
How do you fix oral HPV?

Oral HPV infections can present a spectrum of outcomes, from asymptomatic cases that resolve spontaneously to severe complications such as oral cancers. For many, the infection clears without intervention, but in some instances, it can lead to persistent lesions or tumors in the mouth and throat.
Examples:
- Take, for example, John, a 45-year-old smoker who ignored a persistent sore throat, only to discover a late-stage oral cancer caused by an HPV infection.
- On the other hand, Sarah, a 30-year-old non-smoker, experienced a transient HPV infection that cleared within a few months without any noticeable symptoms.
As we said, getting healthy habits like avoiding tobacco, maintaining good hygiene, and getting vaccinated can help reduce the risk. By staying informed and proactive about oral health, I think you can take steps to mitigate the impact of HPV infections and safeguard their well-being.
What can be mistaken for oral HPV?
Oral thrush
Oral thrush is a fungal infection caused by Candida yeast that can result in white patches or lesions in the mouth, similar to the appearance of some oral HPV lesions. It occurs in individuals with weakened immune systems or those who have taken antibiotics recently.
Oral lichen planus
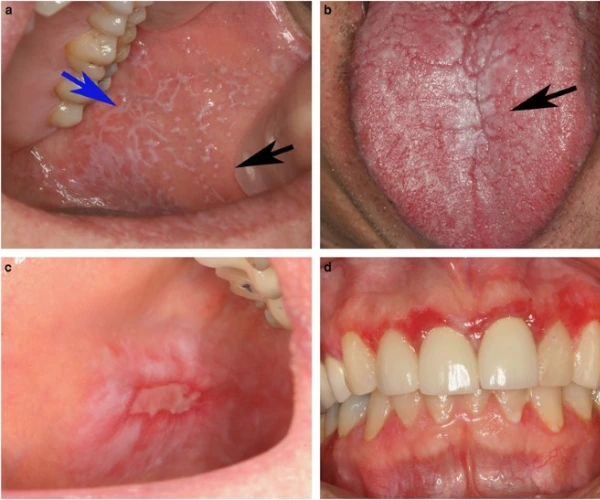
This chronic inflammatory condition can manifest as white, lacy patches or sores in the mouth. It is thought to be an autoimmune disorder and may require treatment to manage symptoms and prevent complications.
Canker sores
Canker sores are shallow, painful ulcers that can develop on the inside of the mouth, often confused with oral HPV lesions. Unlike HPV-related lesions, canker sores are not caused by viral infections and typically heal on their own within a week or two.
What doctor treats oral HPV?
- Oral HPV infections are usually diagnosed by healthcare professionals such as dentists, oral surgeons, or otolaryngologists (ear, nose, and throat specialists). And pros will help manage it.
- Dentists play a vital role in conducting oral examinations, screening for signs of HPV-related lesions, and providing guidance on preventive measures.
- In cases where oral lesions or tumors are detected, oral surgeons or otolaryngologists may perform biopsies or coordinate with oncologists for further management, especially if oral cancer is suspected.
- Primary care physicians may also be involved in the evaluation and referral process for individuals with oral HPV infections.